An Orphaned Disease Worth Adopting: The Case For Duchenne Muscular Dystrophy
Abstract
Duchenne Muscular Dystrophy (DMD) is an incurable disease that kills most of its subjects by their early twenties. This paper examines the need for funding and research of rare diseases like DMD. The National Institute of Health only spends 0.02% of its funding on a disease that affects 30,000 children in the United States (“Estimates of funding,” 2013). This disease is degenerative, destructive, and urgently underfunded. The majority of research is instead funneled into diseases that affect larger portions of the population but also already have effective treatments. Investing in rare or orphan diseases like DMD would yield greater returns than other diseases because research on many common diseases has become over-saturated and can only make incremental progress. Furthermore, there are promising treatments for DMD currently in trial that lack the funding to move forward (Cohen et al., 2012), and there is an untold physical and emotional toll on DMD sufferers and their loved ones because they have no recourse for DMD-specific treatment and are left to struggle on their own. It is imperative that we funnel more funds into a cure that could be on the horizon, and help give these patients and families hope.
Introduction
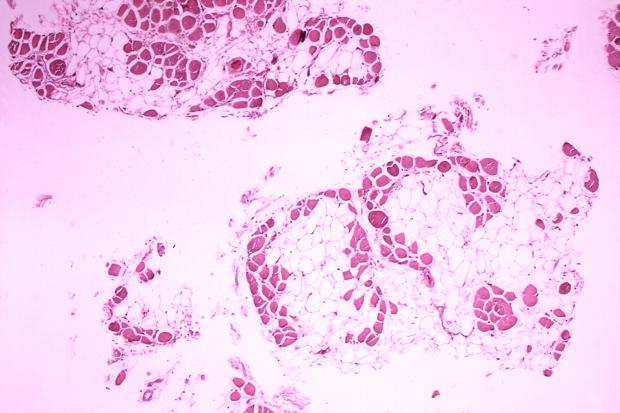
Duchenne Muscular Dystrophy (DMD) is a rare genetic disease that is currently incurable. It is an X-linked recessive disorder primarily affecting young males that causes errors in dystrophin production, a protein necessary for the proper connection and repair of muscle fibers, preventing their muscles from being strengthened. DMD is observed in about 1 in every 3500 live male births, with 35% of cases arising spontaneously without either parent carrying the allele and the other 65% coming from a carrier mother’s affected allele (“About Duchenne,” 2014). DMD can be detected during pregnancy, but most of the time, parents are unaware that their child has the disease until the child is at least five years old. The telltale signs of DMD are difficulty with movement, especially in raising oneself off of the ground. The specific muscular contractions and subsequent movements resulting from this are called Gowers’ manoeuvre (Bushby et al., 2010). Duchenne muscular dystrophy is not well known, despite being the most common form of muscular dystrophy and the most common fatal genetic disorder. In fact, it is the most lethal genetic disorder in children worldwide. Nearly all patients deteriorate and require the aid of a wheelchair and full-time assistance in daily living because of the debilitating nature of the disease. Unfortunately, the vast majority of DMD patients will not live past their twenties. Although there is a huge unmet need, pharmaceutical companies and governments are reluctant to invest more heavily in research because they perceive the cost to be unjustifiable (“About Duchenne,” 2014).
While some consider investment in rare diseases such as DMD a luxury, now is the time to rethink this misguided approach. As a society, we have made tremendous medical progress and have treatments for many common diseases such as hypertension and diabetes. In contrast, there are few options for patients with rare diseases. With recent advances in genetics, novel drug therapy approaches like antisense therapy, exon skipping, and stem cell therapy make finding cures for genetic diseases a reality within our grasp. This cannot happen without strong collaboration between industry and governments. Within rare diseases, DMD is an optimal area to focus funding today. In terms of pharmacoeconomics, industry and governments should divert funds from making incremental improvements for therapies in common diseases to making radical improvements in diseases with no current options, like DMD.
This paper will present a compelling case for investment in rare diseases and DMD in particular. Although I do not know any patients with DMD, I personally know people at GlaxoSmithKline (GSK) who worked hard over the past several years to find a cure for DMD. Unfortunately, the GSK drug failed in Stage III, but it is still being developed by the small biotech company that discovered it. Unlike GSK, this company does not have sufficient funds to continue investigating this promising therapy. I wondered whether the lack of funding would put an end to this treatment. Due to the fact that employee knowledge is prohibited from being shared while they are still working on drug approval with the Food and Drug Administration (FDA), I saw the change in the treatment’s status as an opportunity to learn more about DMD and rare diseases in general. I could not pass up the opportunity to get access to resources and knowledgeable people. Again, I hope to expand the interest in rare diseases and Duchenne especially, as it is exceedingly close to being cured.
There are many published studies on the biological aspects of DMD. In addition, the first cost of illness study for DMD was published in late 2014 (Larkindale et al., 2014). However, since there are no effective treatments, there are no readily available analyses of the pharmacoeconomics of the disease. Studies generally look at the overall impact on the healthcare system of using drug therapies to alleviate the disease burden. My analysis would be the first to prospectively look at the disease as a whole instead of each individual treatment’s benefit over its competitors. It would also determine a range for the value of a new medicine. A drug therapy, in theory, can be expensive as long as it reduces the overall cost of treating a disease while providing benefits to patients, families, and society (Larkindale et al., 2014). The project would also determine the quality adjusted life year (QALY) per dollar invested into DMD in order to allow a comparison to other diseases. These analyses are useful for governments and payers like insurance companies when allocating limited healthcare resources. Currently, the total economic cost of illness for DMD is estimated at $50,953 on average per patient and upwards of $488 million in the United States alone with the acknowledgement that the true burden of illness is likely higher due to the fact explicit costs for DMD treatments are not separated into their own section and that the explicit costs are only the numbers reported by insurance, Medicare, Medicaid, and taxes (Larkindale et al., 2014). While QALY to cost ratios are not perfect, they help encapsulate the impact that each dollar invested has and, as such, are a useful measure in determining the best overall use of funds.
I hope to become involved in research to improve treatments for DMD, specifically its pharmacoeconomic dimension by analyzing the evaluation of the costs and effects of a pharmaceutical drug compared to another drug’s evaluation. Consultants do this currently for individual drugs, but not for DMD as a whole. Marginal benefits are an integral part of the case for investing in diseases like DMD because cumulative benefit is not as important as the improvements per additional capital invested in pharmaceutical development (Davies et al., 2012). Of course, some benefits such as personal satisfaction do not have direct monetary value. Improvement in patients’ quality of life can be included as well via weighing select criteria that are each rated by the patient and doctor, such as treatment safety and social impact on daily lives (Sussex et al., 2013). Ideally, the QALY aspects and financial aspects would be considered in a way that is able to convey the dire need for financial help right now.
I anticipate that the reader will be exposed to the cost-benefit analysis of pharmaceutical drugs, the reasons why Duchenne is biologically close to a cure and how treatments for it could be modified for use on other rare genetic disorders, the current issue of unbalanced resource allocation in drug treatments, the limitations of current DMD research, and why funding is the only hurdle left for DMD to be cured. This article will examine these issues in greater detail.
Resource Allocation
Research on diseases overall could be managed more efficiently to better allocate funds. A contributing factor is the emphasis on certain well-known diseases, which drains resources from other causes. For example, in 2012, the National Institute of Health (NIH) spent $34 million on DMD and $219 million on pediatric AIDS (“Estimates of funding,” 2013). This is despite the fact that pediatric AIDS impacts around 3,000 children in the United States as opposed to 18,000 with DMD (Pediatric HIV and AIDS 2011). Funding in the NIH for each health issue is given based on the perceived needs of a project and the number of projects and is up to the discretion of bureaucratic practices to determine funding. Reforming the NIH to look past public appeal as an important factor would be difficult, but not impossible. Interestingly, since 2009, the first year that appears in the table, funding for pediatric AIDS has fluctuated between $219 million and $228 million, while DMD funding is gradually rising ever so slightly, from $27 million in 2009 to a projected $35 million for fiscal year 2014. While research dollars from the NIH have increased about 11% overall since 2009, DMD’s funds from the NIH have increased 29%, almost 2.7 times more than the average. Thus, at the very least, there is some implicit recognition that research dollars are better invested in DMD than on something else by increasing its funding at such a high rate. However, DMD research still accounts for just 0.02% of total funding of all 235 health issues listed (“Estimates of funding,” 2013). Clearly, DMD is severely underfunded.
In terms of human resources, there is also a disproportionate emphasis on common diseases, with a drain of talent for rare diseases. Society is supporting the development of incremental improvements on existing treatments for diseases that affect many rather than looking for options where none exist. Assuming there is a saturation point whereby improvements are increasingly difficult to achieve, these resources could instead be used for DMD and other rare diseases. As such, 35% of new pharmaceutical drugs approved by the FDA are for rare diseases, despite the fact that they receive significantly less interest and funding than more common diseases (Melnikova, 2012). Thus, a substantially larger share of current drugs being approved per dollar is for rare diseases like DMD, where substantial growth and improvements can be made. Some question whether a rare disease bubble exists, as the actual demand is potentially significantly smaller than the investment, which could signify that this current growth is unsustainable (Merrill, 2012). Even if a bubble does exist, I believe that whether investing in diseases like DMD has popular support or not, it still merits increased funds and does not make investing in treatments for DMD any less necessary. Fear of a bubble bursting on a small project is unheard of and, for other medical missions like cancer research, this is never brought up, nor should it be. Fear of investment hinders progress.
Current Treatments
As of right now, there is a noticeable divide between the percent of patients who elect to receive treatment compared to non-orphan diseases (Cohen et al., 2014). Having not even one DMD-specific treatment likely has had an impact on the rate of participation. Fortunately, there are several drugs in trial. However, many require additional funds to move beyond Stage I or Stage II (Cohen et al., 2014). They vary in risk, with two methods isolated as the options with the least potential risk. The first, exon skipping, allows users to alter their DNA to produce a slightly more functional version of Duchenne, while utrophin upregulation maximizes the production of utrophin, a protein that has 70% homology with dystrophin and serves some similar functions in binding to actin proteins (Malik et al., 2012). Additionally, according to Malik et al., utrophin is so similar that it could help patients with DMD improve their conditions to those of Becker muscular dystrophy, a form that, although equally fatal, adds a few years onto a patient’s life.
Effects and Cost of DMD
The need for treatment is evident in its cost. Having no known treatment, one could expect healthcare costs to be quite low. However, the reality is entirely the reverse. As the health of the patient deteriorates, so too does the caregiver’s state of health (Baiardini et al., 2011). Although not a direct effect of Duchenne, the caregiver’s sacrifice provides an avenue of economic and psychological drain. One-third even suspended their occupation by retiring, resigning, or staying home as a housewife (Baiardini et al., 2011). Studies done on the stress levels and prevalence of mental fatigue and disorders among caregivers find that compared to non-caregiving parents, caregivers report to be significantly more affected mentally by the debilitative process than even their children who have the disease. Self-esteem and mental health overall are reported to be affected, but statistically are not drastically different from normal parent populations. However, social or emotional limitations, general health perception, change in health, and emotional impact on the parent caregiver are all statistically significant enough to be areas of particular concern as secondary effects of having a child with DMD (Baiardini et al., 2011). While there is data now to support the notion that Duchenne muscular dystrophy has a profound impact on the mental health of the caregiver, it is important to recognize that this is not a singular attribute of DMD. The more a parent puts into supporting his or her child, the longer the child tends to live and the less the caregiver tends to live. It should not be this way. With an effective treatment, along with diet and physical therapy sessions, patients would be in a better position to physically move by themselves, relieving some of the stress on the caregiver. According to Bushby et al. (2010), through a strong regimen of stretching and other physical therapy sessions along with a proper and balanced diet program, years can be added onto a patient’s life. More intensive care and higher emphasis on a patient’s diet are cited as reasons for recent rapid changes in the life expectancy of those afflicted with DMD, but the margin of growth is growing slimmer and slimmer each year. There is only so much that can be done before the biologically necessary processes override a patient’s will and determination.
During the last 10 years, the pharmaceutical industry has recognized that investment in rare diseases makes sense. Even in the research and development (R&D) phase, funding is significantly more effective compared to common drugs, encouraging further investment in orphan drugs. For example, according to pharmaceutical industry proponents like Shkreli:
[I]nvestors love orphan drug companies… you can play the upside of pharmaceuticals without having to play the downside of spending hundreds of millions of dollars on R&D. You can get an orphan drug approved for $25 million or $50 million. You don’t have to spend $800 million or $1 billion and spend 10 years waiting for the results (Merrill, 2012).
The large sums of money saved by these smaller operations and time saved provide a wealth of other opportunities to be pursued. Included in this is investing in multiple drug trials for the price of one common drug. Although the profit is guaranteed to be minimal or a loss, this system facilitates quicker and better access to experimental and later approved treatments to help people with rare diseases such as DMD. The pharmaceutical industry is recognizing the opportunity in rare diseases yet the vast majority of R&D budgets are still focused on major diseases like diabetes and hypertension, which are more profitable.
Limitations of Current Methods
Although the current methods of research rely heavily on investment that at first glance appears unstable, the advances made would not be possible without these attempts. The age-old argument of utilitarianism in pharmaceuticals is something that many researchers have tackled, with increasing success. Orphan drugs were named as such due to the fact that they do not make any money because of a small potential market. The more treatments for other diseases improve without improvement in rare diseases, the more logical it is for money to be invested in rare diseases (Davies et al., 2012). Some cautious investors have stayed away from orphan drugs, fearing them to be a bubble market (Merrill, 2012). At the same time, there are optimists who see the recent advances in technology as a sign that we are closer to cures. European governments tend to invest more per person than the United States government does, leading companies to test trials across the pond rather than here (Schmid et al., 2009). Physical location for many more common diseases is not quite as important, as patients have little difficulty with movement and transportation. The limitations imposed upon those with DMD, who must travel by wheelchair and with an accompanying helper, provide challenges that make interconnected, densely populated areas with more government-backed financial support like the Netherlands and the United Kingdom better areas to run trials (Schmid et al., 2009). This is not to say that government needs to finance DMD treatments or trials, but it is a stimulus that will get companies to locate and help people, and make further progress in DMD.
Another reason progress is not quite as fast as anticipated is the lack of information on DMD and rare diseases. With proper data collected, DMD could be compared statistically and comparatively to other, more common diseases. In fact, a lack of data on the exact population of people afflicted with DMD is the reason why potential economic impact ranges from $362 million to $488 million. These types of multi-criteria analyses used to calculate the burden or impact of a disease are relatively recent and evolve as methods improve (Sussex et al., 2013). Many have tried to transform arguably subjective data into quantitative analysis, but none so far has had universal acceptance. The balance between quality of life perception and data collected on muscular ability are finely intertwined, and at the same time it is difficult to determine which is more important. Another controversy is whether quality of life should be quantified in units such as QALY and how far the impact of the disease extends, such as including caregiver detriment in calculations of cost (Baiardini et al., 2011).
The difficulty in investing in rare diseases is that there are literally thousands of diseases with no options, providing an ample array of diseases to profoundly impact upon rather than trying to upgrade treatments for diseases that already have many options. Science and technology advances can help focus efforts on those that are closer to a cure. Specifically, the biological aspects of the causes of DMD are already known, so all that remains is money to fund the various methods with which the biological issue can be dealt. Just 10% of rare diseases have access to any form of treatment, in spite of the fact that an estimated 10% of people have a rare disease (Melnikova, 2012). There is one simple reason why people with DMD have drastically different muscular abilities. One gene, the longest protein-coding gene, just so happens to be the gene responsible for producing dystrophin (Moran, 2012). About 10-15% of cases of DMD occur due to nonsense mutations whereby a stop codon is produced, resulting in less functional proteins (Moran, 2012). Exon skipping technology helps in trying to turn dysfunctional dystrophin into a slightly more functional form by cutting out stop codons (Malik et al., 2012). Additionally, there is a similar protein called utrophin, which has 70% homology, or sequence matching, with dystrophin and is naturally produced at higher levels in the absence of dystrophin that could be used as a surrogate protein in the cytoskeletal matrix (Malik et al., 2012). Exon skipping and utrophin are considered the lowest risk and potentially most effective treatments as of now (Malik et al., 2012). Prosensa/GSK and PTC Therapeutics are currently investigating this exon skipping approach for DMD. Other approaches like gene therapy were once the focus, but now are generally not focused on much due to the risk of causing the patient to develop a form of cancer in the vector transfer of the gene (Malik et al., 2012). The fact that DMD only affects one gene makes it an ideal candidate for any kind of genetic treatment and if and when a cure is found, it could quickly be used as a template for other single-gene disorders.
Conclusion
Finding a cure could save the lives of thousands of people with DMD and thus they could experience life beyond the confines of their wheelchair and potentially live beyond their twenties. Ideally, through continued research, I would have the material necessary to pharmacoeconomically prove that DMD is a good investment based on the improvement it provides per amount of capital invested. However, with so little research and material on which to form an opinion, the QALY to dollar ratio is inaccurate compared to what I would anticipate having in the future with sufficient data. Along with each individual treatment, data would need to be produced to see what improvement it has over the previous treatments and the marginal benefit of investing in it.
The case to invest in rare diseases, and particularly in DMD, is supported by not only the humanitarian arguments of finding treatments or cures for those with no options, but also the economics of the situation. Rightly so, society, governments, industry, and the healthcare system have focused their efforts to combat the major diseases that affect millions of people. Fortunately, we have effective options for most if not all major diseases. It is time to refocus our efforts on the rare or orphan diseases that combined actually affect a greater portion of people than a major disease like diabetes. While finding individual treatments for each is perhaps a daunting task, greater investment can give sufferers of orphan diseases a greater promise for a cure. DMD represents such an opportunity. Patients with rare diseases have been waiting too long. The time to act is now.
Sources
About duchenne. 2014. Parent Project Muscular Dystrophy [Internet]. [cited 2014 Mar 15]. http://www.parentprojectmd.org/site/PageServer?pagename=understand_about.
Baiardini, I, et al. 2011. Quality of life in Duchenne muscular dystrophy: the subjective impact on children and parents. Journal of Child Neurol;26(1):707-713. http://jcn.sagepub.com/content/26/6/707.
Bushby K, Finkel R, Birnkrant DJ, Case LE, Clemens R et al. 2010. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and pharmacological and psychosocial management. The Lancet Neurology;9(1):77-93. http://www.sciencedirect.com/science/article/pii/S1474442209702716.
Cohen JP, Felix A. 2014. Are payers treating orphan drugs differently? Journal of Market Access & Health Policy [Internet]. [cited 2014 Mar 24];2(1):40-44. http://www.jmahp.net/index.php/jmahp/article/view/23513.
Davies JE, Neidle S, Taylor DG. 2012. Developing and paying for medicines for orphan indications in oncology: utilitarian regulation vs equitable care? British Journal of Cancer;106(1):14-17. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3251875/
Estimates of funding for various research, condition, and disease categories (RCDC). 2013. National Institute of Health [Internet]. [cited 2014 Mar 15]. http://report.nih.gov/categorical_spending.aspx.
Larkindale J, Yang W, Hogan PF, Simon CJ, Zhang Y, Jain A, Habeeb-Louks EM, Kennedy A, Cwik VA. 2014. Cost of illness for neuromuscular diseases in the United States. Muscle Nerve;49(3):431-438. onlinelibrary.wiley.com/doi/10.1002/mus.23942/full.
Malik V, Rodino-Klapac L, Mendell JR. 2012. Emerging drugs for duchenne muscular dystrophy. Expert Opinion on Emerging Drugs;17(2):261-277. Available from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3486431/.
Melnikova I. 2012. Rare diseases and orphan drugs. Nature Reviews Drug Discovery [Internet]. [cited 2014 Jan 16];11(1):267-268. Available from http://www.nature.com/nrd/journal/v11/n4/full/nrd3654.html.
Merrill J. 2012. The orphan drug boom: gold rush or flash in the pan? IN VIVO [Internet]. [cited 2014 Jan 20];30(10):1-17. Available from http://www.elsevierbi.com/publications/in-vivo/30/10/the-orphan-drug.
Moran N. 2012. Big players jostle for pole position in muscular dystrophy. Nature Biotechnology [Internet]. [cited 2014 Jan 15];30(10):904-5. http://www.nature.com/nbt/journal/v30/n10/full/nbt1012-904b.html.
Pediatric HIV and AIDS. 2011. U.S. Department of Health and Human Services, Health. Resources and Services Administration, Maternal and Child Health Bureau [Internet]. Rockville, Maryland. [cited 2014 Mar 15].http://mchb.hrsa.gov/chusa11/hstat/hsc/pages/210pha.html.
Schmid EF, Ashkenazy R, Merson J, Smith DA. 2009. Will biomedical innovation change the future of healthcare? Drug Discovery Today;14(21-22):1037-1044. http://www.ncbi.nlm.nih.gov/pubmed/19647096.
Sussex J, Rollet P, Garau M, Schmitt C, Kent A, Hutchings A. 2013. A pilot study of multicriteria decision analysis for valuing orphan medicines. Value in Health;16(8):1163-1169. http://www.sciencedirect.com/science/article/pii/S1098301513043568.
