Can We Grow Replacement Organs? A Survey of Current Literature
Abstract
Although written a century ago, Mary Shelley’s Frankenstein is not far off from the ideas some scientists have for modern medicine. Regenerative medicine, also known as tissue engineering, could be one of the most powerful medical fields in the future. Presently, a donor is usually required when an organ is transplanted. While these transplants frequently result in success stories, issues still persist, predominantly the constant shortage of donated organs. Growing out of this unmet demand is the work of a group of enthusiastic scientists – they have developed a new method of transplantation that obviates the need for a human donor. Instead, the new organ would grow from the patient’s own extracted cells, thereby circumventing not only the current shortages but also the risk for organ rejection. This developing technology has the potential to completely eliminate the main practical and concerns involved in donor-patient transplants, but for some also raises ethical questions. This article will survey conclusions from recent research show new capabilities and high promises for this revolutionary field of medicine.
Although written a century ago, Mary Shelley’s Frankenstein is not far off from the ideas some scientists have for modern medicine. Regenerative medicine, also known as tissue engineering, could be one of the most powerful medical fields in the future. Presently, a donor is usually required when an organ is transplanted. While these transplants frequently result in success stories, issues still persist, predominantly the constant shortage of donated organs. Growing out of this unmet demand is the work of a group of enthusiastic scientists – they have developed a new method of transplantation that obviates the need for a human donor. Instead, the new organ would grow from the patient’s own extracted cells, thereby circumventing not only the current shortages but also the risk for organ rejection. This developing technology has the potential to completely eliminate the main practical and concerns involved in donor-patient transplants, but for some also raises ethical questions. This article will survey conclusions from recent research show new capabilities and high promises for this revolutionary field of medicine.
Risks and Complications Associated with Traditional Organ Transplants
As of December 2009, around 110,000 patients were waiting on long lists for organ transplants (Lee 1). In May, less than half a year later, it was recorded that there were around 2,000 donors. This ratio leaves fifty-five people without organs for every one who finds a match. Even for that one patient who is fortunate enough to receive a matching organ, he or she still faces a winding road to good health. For one, organs must be preserved meticulously, and even when every precaution is taken, organs harvest from a live donor can only be stored for a few hours creating a host of logistical and clinical challenges (Lee 1).
Immunosuppression, a treatment required during organ transplant procedures, poses further risks to the patient post transplant. This process shuts down part of the immune system to lessen the possibility of the body’s rejection of what it considers a foreign and potentially threatening object. Serious side effects are associated with the effects of immunosuppressive medication. For example, improper dosage can cause what is known as oversuppression, a condition which debilitates the immune system so much that the patient cannot even defend himself against generic pathogens, leading to frequent and sometimes serious infections (Lee 1).
In light of these concerns in addition to the shortage of organs, the rationale for biomedical engineers and medical doctors are shifting their attention and hopes to tissue engineering is clear. This new and exciting science keeps those studying it enthusiastic and eager to perfect the technology in order to fully reap all its potential benefits (Lee 1).
Pioneers of Regenerative Medicine
The three main pioneers who first investigated the idea of tissue engineering twenty-five years ago were brothers Joseph and Charles Vacanti, of Harvard Medicine, and Robert Langer, of the Massachusetts Institute of Technology. Based on clinical research, these researchers concluded that organ and tissue regeneration consisted of three basic steps: 1. Scaffolding, 2. Laying cells, and 3. Implantation (Komaroff, 56).
Scaffolding
The scaffolding for organ regeneration is the first step in the process. Using biodegradable materials, cells are laid onto a model organ. This scaffolding serves as a platform for growth and specifies the pattern in which the cells will develop, depending on the target tissue. The key concern with scaffolding is how the structure will break down cleanly when the time comes. Research has led scientists to select collagen, a fibrous protein found in structural tissues, as a suitable material for constructing the scaffold. This material holds well throughout the growing process, but as the organ takes shape and assumes function, it breaks down without complications (Aschiem, 1311).
Laying Cells
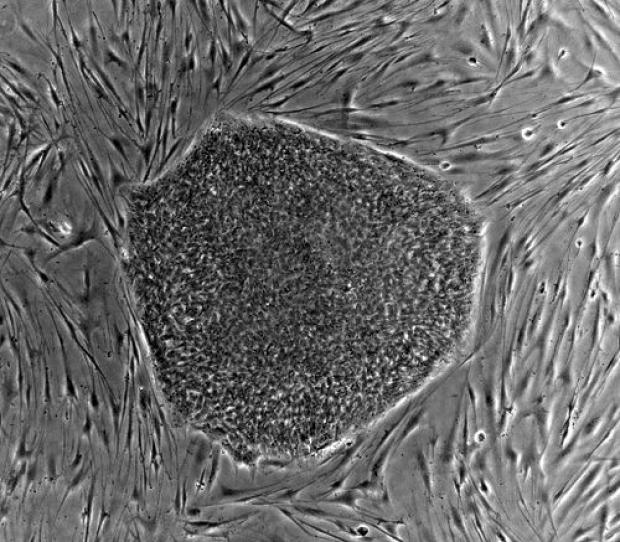
Once the scaffolding is set up, living cells are introduce in the second step of the process. Described by Dr. Anthony Atala as “much like baking a cake,” this step involves laying stem cells (harvested directly from the patient) down evenly across the collagen (60 Minutes). The cells are draped gently in small layers, setting the stage for growth. These cells are then cultured in incubators that simulate the human body in temperature, carbon dioxide and oxygen levels, among other environmental characteristics, in order for the cells to grow as naturally as possible.
After six to eight weeks of growth in the simulated external environment, the growing cells that will become the replacement organ are re-introduced into the patient’s body (Orlando 1011). Although transplantation is by then complete, the organ is not yet fully mature. The partially grown organ is placed onto its doppelganger, the dysfunctional original (Aschiem, 1311).
Implantation
This transfer from an external incubator back into the body is crucial for the new organ’s vascular development, such as that of arteries, veins, and capillaries. Vascular tissue allows for gas exchange, which in turn acts as the motor for cellular respiration, giving cells oxygen and removing carbon dioxide as they produce the energy necessary to survive. Only placed in its rightful place, surrounded by the right tissues in the body, can the new organ know to start vascularization; place-specific signals modify the genetic expression of the organ’s cells so they can further develop into specialized tissues. “If you place a cell in the right environment it will know what to do,” stated Dr. Atala (60 Minutes). These developmental signals are absent in man-made incubators, despited the simulation of other environmental characteristics as previously described.
Within three months the organ grows to approximately two-thirds of its final size and shape, and within six months, a new and fully functioning organ is present, thus completing the procedure. By this point, the scaffolding needed to support the cells during the initial stage of growth will have completely degraded. With the new organ in place, the unhealthy organ can be safely removed.
The Use of Stem Cells
While the benefits of regenerative medicing for tissue engineering are numerous, one factor that has prompted ethical questions about this innovative science was its initial use of embryonic stem cells. The process by which this type of stem cell was obtained sparked a long and aggressive controversy. As an embryo develops, stem cells replicate, eventually differentiating into adult cells with specific functions (called somatic cells). Obtaining embryonic stem cells requires unnaturally ending the growth process of an embryo, which some consider to be the destruction of life. The opposing side argues that life has not yet started at this stage of development. Irregardless, today a government ban prohibits funding for embryonic stem cell research. This could have led scientists to suspend or abandon research on innovative and life saving procedures such as the kind of tissue engineering described above.
Fortunately, recent developments in regenerative medicine have eliminated these ethical concerns and allowed this important research to continue. While it is true that in the earliest attempts to grow replacement organs embryonic stem cells were thought to be the only way to reconstruct a new organ, partially as a result of the aforementioned government ban more recent research has demonstrated the efficacy of another kind of stems cells: somatic cells. The use of these cells, harvested directly from the patient and then used to regrow the necessary organ, has led to major scientific breakthroughs in regenerative medicine while avoiding the ethical dilemma posed by the use of embryonic stem cells. For example, in the first tissue-engineered bladder transplants by Dr. Atala, autologous cells were seeded on matrices. In an autologous procedure the patient’s own cells, in this case urothelial and muscle cells, are surgically obtained, replicated in culture, and seeded on biodegradable bladder scaffolding for growth.
Follow-up reports on ten of Dr. Atala’s patients who underwent this procedure demonstrate adequate structure and function with no significant complications (Orlando, 1011). The results of Dr. Atala’s successful attempts to regrow and transplant bladders using autologous stem cells showed that embryonic stem cells were not necessary to regrow particular organs in a lab. The published findings encouraged other scientists to experiment and pursue research beyond embryonic stem cell use for regenerative medicine.
While early procedures were performed using somatic cells, autologous stem cells are now thought to be much more favorable for their longer life span and flexibility in development (Peterson, 3751). Somatic cells eventually enter what is known as replicative dissonance, meaning they are unable to replicate anymore. Recently, scientists have been experimenting with other types of cells that, like autologous stem cells, such as induced pluripotent stem cells, the type present in adult bodies. Unlike embryonic stem cells, these need not involve interfering with embryonic development and thus raise fewer ethical questions.
Model Procedures
Dr. Atala is one of the major pioneers in the field of tissue engineering. He is also considered the face of regenerative medicine as he has been featured in various news segments including 60 Minutes. After medical school, Atala worked in the urology department of the Children’s Hospital in Boston, where he noticed the consequences of transplant organ shortages around the world (Aschiem 1311). He soon transferred to Wake Forest University in Winston-Salem, North Carolina, only seventy-five miles from UNC, where he remains today as Director of the Institute for Regenerative Medicine.
While his advancements are extensive, Dr. Atala is most known for his experimental procedures on ten bladder-transplant patients, who are living healthy lives more than forty-six months later (Orlando 1012). He conducted the first human trial using tissue-engineered organs and paved the road for regenerative medicine across the globe. As a world leader in the field of regenerative medicie, Atala’s department is pursuing new applications for his research including tissue-engineered urethras, blood vessels, cartilage, muscle, bone, kidneys, and tracheas (Aschiem 1311).
Another scientist, Dr. Tracy Grikscheit, has also been making pioneering steps in regenerative medicine. While specializing in Short Bowel Syndrome, she began conducting research on tissue engineering in pursuit of a cure for the condition (Komaroff 56). Short Bowel Syndrome is a congenital condition where the small intestine is too short for adequate absorption of nutrients during digestion. Grikscheit has developed the proper procedure and scaffolding to produce short sections of the small intestine to add to the patient’s body. She has successfully performed the full procedure on pigs, in which the new intestinal segments adopted full circulatory function and its own nerve supply. The success of these trials, Grikscheit hopes, will pave the way for human trials similar to those performed by Atala.
One of the most enthusiastic supporters of regenerative medicine is the military. Thousands of soldiers return home missing extremities. Josh Maloney, for example, is a soldier whose right hand was injured during a training exercise. His injury led to amputation (60 Minutes). At first, the young man thought he would continue his life wholly dependent on his left hand; however, thanks to new tissue engineering technology, Josh was presented with an unusual opportunity to get a new right hand.
Doctors at the University of Pittsburg successfully transplanted the hand from a cadaver using various cell therapy techniques along with a bone marrow transplant. In a similar manner, Machiarini and Walles conducted a procedure in which a thirty year-old woman received a bioengineered human trachea (Orlando1012). The scaffolding, also obtained from a cadaver, was draped with autologous cells mainly derived from mesenchymal stem cells and epithelial cells. As of a four-month follow-up, Machiarini and Walles’ patient was in stable conditions and no immunosuppression was necessary. The success of these early attempts to replace organs, and in the case of Josh Maloney a hand, open up new possibilities for the potentials of regenerative medicine. Soldiers, young men and women who fight for our freedom, may one day be able to replace full limbs lost in battle.
Conclusion
Autologous stem cells evade the technical problems posed by somatic cells, and induced pluripotent stem cells avoid the ethical concerns embryonic stem cells present. The advancements in this technology as a whole are promising. Yet, four key issues remain pressing: advances in scaffolding, research into the benefits of different types of cells, post-transplant regulation, and funding (Orlando 1012). Among these concerns, proper funding is perhaps the most critical as it will allow scientists to not only perform these lifesaving procedures in small clinical trials, but to develop efficient ways to monitor patients afterwards, and develop research to expand the current applications. Health and quality of life are what doctors want to guarantee their patients. The advancement of tissue engineering poses a very real and promising step towards fulfilling this mission.
Sources
Orlando, G. et al “Regenerative Medicine Applied to Solid Organ Transplantation: Where Do We Stand?” Transplantation Proceedings 42.4 (2010): 1011-1013. Print.
Petersen, Thomas, and Laura Niklason “Cellular Lifespan and Regenerative Medicine.” Biomaterials 28.28 (2007): 3751-3756. Print.
Chung, Young et al “Reprogramming of Human Somatic Cells Using Human and Animal Oocytes.” Cloning and Stem Cells 11.2 (2009): 213-223. Print.
Denker, Dr Hans-Werner. “Induced Pluripotent Stem Cells: How to Deal with the
Developmental Potential.” Reproductive Biomedecine Online 19.1 (2009): 34-37. Print.
Aschheim, Kathy. “Anthony Atala.” Nature Biotechnology 24.11 (2006): 1311. Web. 18 Jan. 2010.
Komaroff, Anthony L. “The race to grow new organs.” Newsweek 13 Dec. 2010: 56. Academic OneFile. Web. 22 Feb. 2011.
Orlando, Giuseppe et al “Regenerative Medicine as Applied to Solid Organ Transplantation: Current
Status and Future Challenges.” Transplant Internaional 24.3 (2011): 223-232. Print.
N, Jallali et al “The Current Role of Tissue Engineering in Head and Neck Reconstruction.” Indian Journal of Cancer 47.3 (2010): 274-279. Print.
Imaizumi, Mitsuyoshi et al “Potential of Induced Pluripotent Stem Cells for Regeneration of the Tracheal Wall.” Annals of Otology, Rhinology & Larygology 119.10 (2010): 697-703. Print.
Lee, Anthony Suite 101. 29 Mar. 2008. 22 Feb. 2011 <http://www.suite101.com/content/issues-with-organ-transplants-a49167>.
