The Wrong Diagnosis: Why Infectious Disease Continues to Undermine Africa’s Development
Abstract
Infectious disease is a part of the human existence, a necessary experience which is shared by people from all walks of life. In the developed world, illnesses such as the common cold come and go with relatively little impact on the people they touch. Adults must suffer to take a few days off from work while children delightedly miss a day or two of school, but in almost all cases the patients bounce back quickly and their lives return to normal. In the developing world, especially Africa, the situation is radically different; pervasive infectious disease and its detrimental impacts on daily life are a constant crisis rather than a passing nuisance. On a larger scale, its accumulated effects on the inhabitants of Africa have coalesced into a much more serious picture of stunted growth and development across the continent. In this paper, Chris Rota explores both how disease has affected African development as well as the equally important reciprocal effect which the slowing of development has had on perpetuating its disease problem. The essay is divided into several sections: the first is a brief introduction to Africa and its diseases while the second discusses the current situation of Africa, both in how disease affects the daily lives of its people and in how insufficient medical treatment and overall infrastructure are exacerbating these conditions. The third and fourth sections address the economic and political forces, respectively, causing the infrastructure end of the issue and raise points which global institutions should take into account as they continue to make efforts to solve the crisis in the near future.
Introduction
The opening decades of the 20th century marked the end of colonial empires around the world. However, as world war has given way to world integration and rapid global development, Africa has consistently fallen behind in both the pace and scope of its modernization. While the populace of the more developed nations lives in relative comfort, millions of deaths each year in the African countries continue to arise from preventable factors such as inadequate nutrition, lack of clean water availability, medical complications during childbirth, and communicable disease (Millennium 2). Individually, each of these problems represents a serious pitfall to the health of their respective communities; therefore, as a group they can become a nearly insurmountable challenge. The absence of a proper diet and clean water can cause increased disease, which spreads thin local medical infrastructure and places financial burden on families without members to work and bring home income. Because money is scarce the funds to purchase proper water purifiers and supply a balanced diet disappears as well, beginning the vicious cycle anew. Though not always in this same form, nearly all the stories of development in the nations of the Sub-Saharan African region have come to a similar ending: a resounding failure to secure the most basic of necessities for all their citizens.
Out of the many factors contributing to this crisis, the persistence of disease among the African population has been one of the most harmful to the region’s economic and political modernization as a whole; tropical diseases such as malaria and tuberculosis still affect well over 100 million people within Sub-Saharan Africa alone and remain the leading causes of death, especially among children (Hotez and Kamath 5). Though the numbers alone are a cause for worry, the most disturbing facet of the problem is that both of the aforementioned diseases are easily treatable with the proper resources. Malaria, for instance, can be handled by proper medical care and the application of basic antibiotics in all but the most severe cases. According to the WHO, the disease claimed a little over a 1000 combined lives in the entire European and American regions (both North and South). In the African region, the same disease claimed nearly 760,000 lives (Health 2008). But they are not the only offenders. Each year, the political and economic systems of these countries condemn millions of individuals to death because they have disconnected the global medical community from the patients who need its care the most. Although the treatment of infectious diseases has improved due to foreign intervention, the overall medical infrastructure of Africa is still extremely inadequate at ensuring the most basic of human rights for its citizens: the right to a healthy and fulfilling life.
The Situation As It Stands
At the beginning of the second millennium, the United Nations adopted an ambitious plan for promoting the growth and advancement of the world’s poorest individuals. Formally termed the Millennium Development Goals, the plan acknowledged and suggested courses of global action to solve the myriad factors which have led to the current situation of this population, a group economist Paul Collier termed, the “bottom billion.” These people are often lumped in among the nearly five billion members of the collective nations of the developing world, but their situation is unique. As Collier himself puts it, “these countries now at the bottom are distinctive not just in being the poorest, but also in having failed to grow…many of these countries are not just falling behind, they are falling apart” (Collier x). Even the most powerful of the developed world countries has fallen prey to economic depression, war, and disease epidemics at some point in its history, but such conditions are fleeting for most countries’ development, the home nations of the bottom billion have endured these conditions for generations without ebb. Insidious diseases, unclean water, poor education, widespread social inequity, constant violence; these and other injustices are the birthright of a child of the bottom billion, to be taken as unchanging and permanent. While others live in comfort, most of these children will live and die in the pit of poverty simply because they were born in the wrong place.
Since the inception of the Millenium Development Goals, global statistics would suggest that progress is being made; a study by Chen and Ravallion in 2004 found that the number of people in extreme poverty decreased from 1.21 billion to 1.09 billion and is likely to continue declining (Millennium 2). However, as the Project recognizes, this and other signs of progress for the developing world as a whole do not tell the entire story. Most notably, they obscure the fact that the majority of Sub-Saharan Africa has failed to make significant progress towards achieving any of the goals, chiefly among them reducing disease spread and mortality. At its heart, this problem is a consequence of the world’s ignorance towards the dynamics of the region and fundamental lack of understanding of how to effectively fight disease in Africa. The economic and political antidotes for developmental stagnation which have worked elsewhere in the globe must be adapted to the region’s unique needs if success is ever going to be achieved.
Infectious disease as a general entity is not exclusively an African problem, but the extent of the disease problem within Africa is itself rather unique. Currently, the most prevalent and harmful infectious disease after AIDS in the African continent is malaria (Rao); as pervasive and equally dire the AIDS situation is, it will not be discussed in this essay (see the footnote at the conclusion of the essay for a more in-depth explanation). This disease is present in many countries around the world and has flourished in rural regions of the continent due to the lack of a coordinated and educated effort to stamp it out. Such interventions are by no means unfeasible; as recently as 2008, a systematic effort to wipe malaria from the island of Sri Lanka has been occurring under the guidance of the Indian government (Abeyasinghe 3). If one government is capable of solving the disease problems of a historically epidemic-ridden island, it would seem logical that a coalition of many governments could solve the disease crisis of Africa. However, foreign aid has historically undershot the necessary levels to produce substantial change, aswith anti-malaria spending for projects in 2002; the total came to only $100 million in U.S dollars, while the WHO estimated that at least several billion dollars would be needed to achieve substantial reductions in the spread of the disease worldwide (Narasimhan 5). Even in good times there is often still failure to achieve results; the World Health Organization said in a 2008 report that despite increases in the supplies of insectide-treated nets and anti-malarial drugs, overall availability of these supplies decreased for the average African (WHO 6). Additionally, the report states that only nine of the forty-six African countries are projected to achieve the Millenium Development goal for reduction of the malaria threat by 2015. This ratio offers evidence that the effort to treat infectious disease in Africa is not evenly spread throughout the region. The global community has tended to concentrate its resources on those countries with lower disease burdens and higher functioning economies, so as to maximize the benefits resulting from disease reduction efforts and produce those benefits in a relatively short amount of time (Tanner 2). In doing so, the small-scale problems are solved but the largest ones in most dire need of aid have gone relatively untreated. Beneath the tales of positive statistics and overall trends of lowering disease spread, diseases such as malaria weigh down large groups of individuals where they are most prevalent and difficult to deal with.
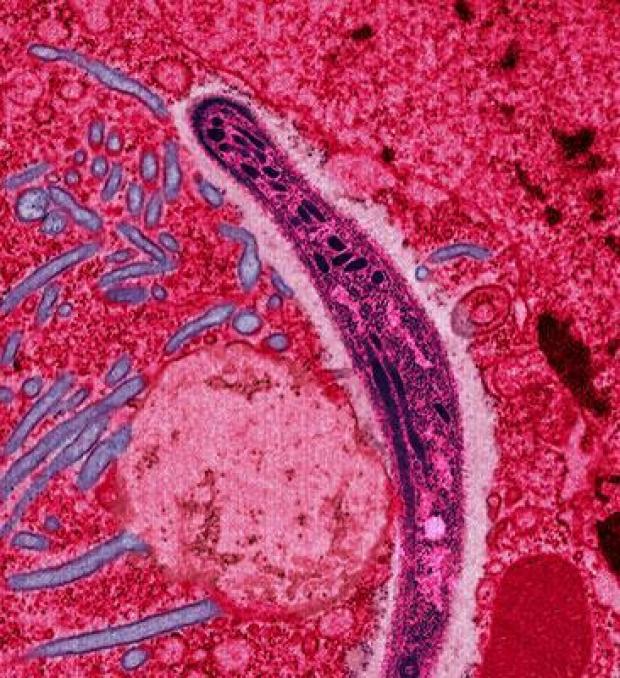
As malaria is the poster child for the African infectious disease threat, a similarly vital underscoring problem has been the development of antibiotic-resistant strains of disease among the rural population. When a population of infectious bacteria is exposed to an antibiotic, they typically expire quickly; however, it is possible that some of these bacteria will have inherent resistances to certain types of antibiotics within their genomes by means of random mutation. These mutants will go on to reproduce and repopulate the host if left unchecked, passing on the resistance to their offspring and leading to a second, even more serious infection. One would think that such an outcome would result from an undertreatment of a disease. In fact, Africa’s problem with antibiotic resistance seems to have resulted from exuberant overtreatment. Prescribers and patients in developing countries have latched onto antibiotics as a solution to a much wider variety of medical problems than they can actually solve, and the pressure to provide these drugs has become a major incentive to ignore the possibility of dangerous side effects such as resistant bacteria strains. For example, a survey conducted in South America found that doctors were afraid to hold out on prescribing antibiotics to patients who appear sick with deadly diseases such as malaria, and thereby be responsible for preventable deaths (Haak 6). However, the reality is that many patients are simply being misdiagnosed by clinics that use only basic physical symptoms and laboratory tests, and end up taking antibiotics when none are truly needed. A study in Ghana found that only 40% of all patients diagnosed with malaria actually had the malaria-causing parasite. (Perri 2). Dutch researchers also found that antibiotic compounds “[are] often being perceived as…capable of curing almost any disease…even reach[ing] magic proportions,” as a result of cultural superstitions, resulting in the massive over usage of antibiotics (Haak 2). Patients’ improper application of the antibiotics compounds this over usage, and leads to, the emergence of resistant bacteria strains. The global medical community’s drive to fight disease outbreak has exacerbated the current health problems of the bottom billion, merely treating their symptoms rather than trying to find the source of the problem.
Once basic antibiotics such as penicillin and tetracycline are no longer effective due to overuse, more powerful and rare ones must be administered to repress the bacterial infections. The discovery and subsequent development of new antibiotics for medical use requires both scientific expertise and extensive laboratory resources, both of which require capital investments that Sub-Saharan African economies can not support. Whereas generic drugs are easily and cheaply imported because the manufacturing methods are well established and patents protecting proprietary formulas have expired, the newest and most effective formulas needed to treat drug-resistant diseases are both expensive and difficult to produce in the necessary quantities for the average African citizen to use (Clardy 3). If the trend of antibiotic over-use is not corrected, outbreaks of resistant “super diseases” will become more frequent and consequently more damaging to the progress being made in bringing rural Africa out of the shadow of disease (Espinal 8). But like a weed, the root of the problem choking its development is buried and not easily reached or treated. On a global scale, the technology and capital resources needed to address many of these preventable life-threatening diseases are plentiful. Yet, the specific local, cultural, political, and economic roots of disease are deeply ingrained throughout the Sub-Saharan region.
Globalization and the Roots of Africa’s Economic Troubles
Globalization, as S.T Akindele states, “refers to the process of the intensification of economic, political, social and cultural relations across international boundaries…[a movement] principally aimed at the transcendental homogenization of political and socio-economic theory” (1). Characterized by the rise of multinational corporations and a large-scale opening of trade channels between nations, this movement has dominated world economic policy since the early parts of the 20th century and led to rapid growth in global economic exchange. In theory, an acceleration of the globe’s economic pace benefits all sides of the equation. Natural resources suppliers can capitalize and create profit more quickly; industrial producers can turn out more products and therefore also increase profit, and the resulting gains from both ends trickle down to the working class. However, the rapaciousness of global development has brought a pressure upon local African governments to quickly pry open the region’s vast troves of resources for usage in world industry, which has retarded the rise of infant industries that occurred in the developed world and led to their current success (Akindele 6). Foreign corporations often take over the lucrative process of extraction due to the expertise and technology required, leading to the formation of economic infrastructure which relies upon foreign aid rather the skills of its own populace (Akindele 4). By forbidding African entrepreneurs and industrial leaders to truly participate in global expansion, the transformation of accumulated capital from large businesses into wealth for the general population and the main avenue for advancing general welfare has been almost closed off. Though global businesses and their customers benefit from the specialization of the African economy, the individual countries that contribute to the system become incentivized to suppress the skill level of the working class (Akindele 3). Over time, this process has created economies, which rely on menial labor and low-end industrial jobs to support themselves, with very few attainable advancement opportunities for the high-achieving individual (Akindele 4). Migration out of these bottom countries will become increasingly skewed towards this latter demographic. As Paul Collier writes, “having already hemorrhaged capital, the countries at the bottom will increasingly hemorrhage educated labor” (Collier 94). The perpetuation of streaming resources and funds through the Africa countries without investing in their development has marginalized them at the bottom of the world’s economic ladder. This legacy of marginalization is one of the primary roots of the disease crisis; without the money or human capital to build up their medical infrastructure, these nations will continue to be placed at the mercy of infectious diseases for the conceivable future.
Additionally, the widespread presence of disease due to a lack of a strong medical infrastructure has had a reciprocal effect on the individual economies of many African countries. Many scientists, notably economist Jeffrey Sachs, have used the term “disease burden”, to describe this phenomenon and entails both economic and social costs for the affected individuals as well as those around them (Sachs 3). The economic aspect is most easily understood as the decrease in productivity resulting from an illness. Between a sick individual and a healthy one, the healthy one will invariably be able to accomplish more tasks with greater efficiency and speed. Sick members of the workforce must also take days off for recovery and spend hard-earned wages on doctor’s visits and medication to fight off the disease (Sachs 2). For a family reliant on a just a few working members, such an event can have a drastic impact on the family’s quality of life. In a study of national income levels across the globe, it was found that “average GDP (adjusted to give parity of purchasing power) in malarious countries in 1995 was US$1,526, compared with US $8,268 in countries without intensive malaria — more than a fivefold difference” (Sachs 2). The household’s overall productivity is often affected as well as other family members must spend time caring for the sick individual, which could put them at risk of also becoming ill.
The social aspect of a country’s disease burden is much harder to quantify than the economic one because it involves the development of individuals and communities and how their actions are altered as a result of the presence of various diseases. This weight falls most heavily on the younger generations. According to Sachs, “in areas of stable, endemic transmission about 25% of all-cause mortality in children aged 0 to 4 has been attributed directly to malaria,” meaning that the percentage of deaths related to all diseases is probably even greater. The results of such early deaths are profound within the context of the African family, as children are a large investment of time and effort on the part of the parents and therefore represent a loss of precious family resources should they die prematurely. It has even been proposed that African parents choose to have more children than they actually desire in case some of them fall to disease (Sachs 3). As callous as it may seem to think of children as material resources rather than people, it is a point of view which illustrates the difficult realities faced by these families. Normal economic costs associated with children, such as purchasing food and clothing, are compounded in the context of poverty; whereas such additional costs are not a tremendous stretch for a middle-class couple in a more developed country, parents in bottom billion countries are likely to be sinking a much more significant amount of their income and savings into raising their children. The magnitude of that investment means that getting a return in the form of a able-bodied child who can generate additional income is all the more crucial, and the lack of a return all the more devastating to the family’s financial future. Another possibility is that the family, anticipating infant mortality due to disease, has more children than they actually desire or are able to support, a trend which was noted by Jeffrey Sachs in his research (3). The uncertainty of such mortality means that the family could end up having no losses at all and wind up facing ruinous economic consequences.
The impact of disease on children’s development is an equally worrisome social trend because disease can prove extremely disruptive to their education. African elementary school students miss almost 1 in 9 days of school per year due to disease (11% of the total class time), which greatly detracts from their learning and hinders their advancement to secondary school and beyond. Just 62% of primary or elementary school students in the whole of Africa continue their education after graduating. In addition, many individual countries graduate under 50%, with the lowest being 21% in Niger (UNESCO). Without an education, these children will be unable to rise out of the working class to higher paying jobs in the future, and quickly become routed into the world of low-income, dead-end jobs from which escape is very difficult if not impossible. Such an economic entrapment often leads to a more physical entrapment as well; low-income families have little to no means to escape from their rural villages and inner city neighborhoods, locations where disease thrives. A vicious cycle ensues, as the following generation becomes born into social conditions which set them on the same course as their parents before them and perpetuate the entrapment. The few individuals who do manage to escape the cycle and become economically successful are faced with a problem, namely how to best safeguard their success for the next generation so as to break the cycle permanently. As previously discussed, the most compelling solution is often to simply leave the country; while such actions have great merit on the scale of the individual, they hold grave consequences for those left behind. The talent which is necessary to solve the disease problem, a crisis facing the entire population, is being pushed away rather than harnessed by the medical sector. It is at this point that the disease problem ceases to be solely an economic one, and also becomes an issue of the state’s ability to provide for its people, both those who have found success and those who have not.
African Politics and the Legacy of Colonialism
Out of all the impacts of globalization, one of its greatest consequences concerning the development of disease has been a mentality of the “eternal state,” which puts the persistence of a regime above the needs of the public. As Tukumbi Lumumba-Kasongo, an African political scientist, states: “Privatization is one of the most important dimensions of the [African] state that has impeded any kind of consensus emerging in relation to… programs of social progress.” (92). He describes a trend that links together the current economic and political situations of Africa: a large-scale, sustained effort to “render the public domain of social life irrelevant” (Lumuba-Kasongo 92). By privatizing the affairs of the state during the colonial era, European colonizers laid the groundwork for creating a culture of political self-service, holding the interests of the government as greater than those of the people. In his own analysis, Collier used the following example to describe the magnitude of the effect of poor governance on solving a nation’s problems:
In 2004 a survey tracked money released by the Ministry of Finance in Chad intended for rural health clinics. The survey had the extremely modest purpose of finding out how much of the money actually reached the clinics – not whether the clinics spent it well or whether the staff of the clinics knew what they were doing, just where the money went. Amazingly, less than 1 percent of it reached the clinics – 99 percent failed to reach its destination.” (66)
Many of the worst offenders in poor governance historically have been authoritarian regimes, such as Nigeria from 1970-1990, which carried on the colonial practice of exploiting public resources to maintain their stranglehold on power (Collier 46). But even in areas where democracy has prevailed over authoritarianism, states such as the Democratic Republic of the Congo have preferred to invest the money garnered from their natural resources in national security and wasteful industrial projects rather than public infrastructure such as schools, hospitals, and medical research facilities.
There are two main reasons why this trend of development has been allowed to occur, both of which are a direct result of the large profit margins associated with natural resources. With high amounts of revenues streaming in, a government can afford to lower its taxation rate on the public, consequently lowering the amount of public scrutiny on how taxes are being spent (Collier 46). The second reason is the existence of patronage politics in some form in the vast majority of resource-rich states, including the Congo. Often, “in the context of ethnic loyalties and the absence of press freedom, patronage politics is more cost-effective than the provision of public services as a strategy for winning elections” (Collier 45). In such a system, votes are won through up-front gifts and promises of direct economic benefits rather than the promise of public investment. Therefore, supporting a patronage-based party is logical on the basis of a single poor African citizen looking to improve their economic standing. Nationally, these choices have taken a disastrous toll on the development of the public sector. Since such development is not a priority for patronage politicians, institutions such as hospitals and medical research facilities have been slowly starved of the funds they need to tackle the crisis of persistent infectious disease. In 2009, the World Bank found that the per-capita health expenditure of the Democratic Republic of the Congo was a measly 16 U.S dollars, with roughly half of that money being contributed by the government (World Bank Data). An single 5 day antibiotic treatment for malaria used in a study in Thailand cost $11.49 (Honrado 4). Because these African governments do not provide the public with the resources necessary to combat disease, they irresponsibly leave their citizens without any reliable means of medical treatment acquisition and little hope for a government-sponsored initiative to address the disease crisis.
Another facet to the political roots of Africa’s disease crisis has been the often overbearing nature of foreign influence, most notably seen through the giving of monetary aid to African governments by foreign entities. Since the end of colonization, the region’s political and economic systems have evolved into a complex rhizomatic network, reliant upon recurring infusions of global financial aid and concomitant political intervention to survive (Bräutigam 1). Repeated injections of capital were meant to boost the economic system and spur positive and sustainable progress. Instead, financial aid programs have become institutionalized, resulting in ongoing economic dependencies and political stagnancy. In 1999 the amount of foreign monetary aid given to Rwanda equaled 99% of its GDP (Bräutigam 5); in essence, the addition of foreign aid doubled the size of the Rwandan economy in terms of money spent on economic transactions. The hidden curse of such elevated levels of economic activity is the necessity of an equally elevated level of government activity within the country to manage the increased volume of economic activity. Foreign aid projects such as the perennially popular building of schools, while desperately needed, nearly always require supervision by the host government. This need is not a problem until the amount of projects exceeds the amount of time government officials have to devote to them. Authority figures of small impoverished countries are becoming increasingly wrapped up in tending to foreign aid providers than actually working towards solving the nation’s problems (Bräutigam 8). By expanding activity far beyond a government’s capabilities, excessive foreign assistance can lead to a dilution of political willpower and development of “servant states” to more powerful private interests. It is easy to see how the disease crisis could go ignored as the government becomes an instrument for accomplishing the bidding of both external and internal puppeteers rather than serving the public good, and how the failure of disease elimination programs not only within individual countries, but within the region as a whole would be virtually guaranteed.
Looking Forward to a Disease-Free Africa
Disease elimination in Africa has been one of the most challenging dilemmas to ever face the global medical infrastructure. The lack of sufficient medical infrastructure to combat the endemic diseases in the region inhibited the success of elimination programs in the past, though such programs for the same diseases succeeded in more industrialized areas such as Europe and North America (Tanner 1). Medicine is far more advanced and well-adapted to deal with disease today than it was in those days, with volumes of research having been performed on developing new antibiotics and countless other methods of dealing with disease. Yet, even with an increase in world resolve to combat disease with the establishment of the Millennium Development Goals, none of these have been successfully implemented. The translation of global medical advancements into progress [everywhere? Or just in the region you’ve been discussing?] has been extremely poor, with global efforts to aid in solving the crisis consistently falling short of their targets: the human beings, individual African patients plagued by an inescapable scourge of disease. On many occasions, Foreign intervention exacerbated the, and our globalizing world has pushed the region of Sub-Saharan Africa to the very fringes of society. Economically, its nations have been crushed beneath the weight of multinational corporations and an equally inescapable past of exploitation both from within and without. Politically, they have suffered from a government warped into a reckless machine that devours public revenues to sustain itself at the cost of the public good. While Africa cannot be expected to independently rise out of the infectious disease shadow, it is clear that the next stages of progress towards control and eventual disease elimination must originate from within the African continent.
As Claude Ake, a well-known African political scholar, once said, “Development is something that people must do for themselves. If people are the end of development, they are also necessarily its agents and its means” (Lumumba-Kasongo 5). Unless the people of Africa are the primary actors in developing their medical infrastructure and changing the mentality of their governance, any advancement made in disease reduction by outside forces will be unsustainable in the long run. Therefore, the goal of current efforts to halt the spread of disease should not be focused on the reduction of the diseases themselves, but on trying to reignite the heart of African development. Creating a well educated population empowered enough to fight local diseases autonomously is the only truly lasting solution to the current crisis. No matter how strong of an antibiotic or treatment the medical community may develop, the hands of each African must be able to obtain it and learn to wield it for themselves before they can win the fight against disease.
A Note on AIDS:
The AIDS/HIV epidemic has been one of the most widely covered disease stories of the 21st century, ingraining itself in the global medical sphere and inspiring donors and activists from around the world. The AIDS story, unlike the story of many other African infectious diseases, has been one with a very positive ending: there has been an enormous turnaround in the treatment and spread of awareness among the African population. Many of the other infectious diseases, including malaria, have gotten much less international attention and donor support and therefore compel me personally more to spread their story. However, the most compelling reason I have for avoiding a discussion of AIDS/HIV in this article is its root causes. While the factors of economics and governance discussed have impacted the pervasiveness of AIDS, they are secondary to the social causes of the disease’s spread. The culture of sexual protection, African family life, African social norms, and the epidemic of sexual assaults in Africa’s conflicts are crucial elements of the story of AIDS but not to the stories of the many infectious diseases I am discussing in the context of this essay. If you do wish to know more about the unique story of AIDS, a great volume of scientific literature exists which can do a much better job of explanation than I ever could in the small space of this essay.
Sources
Abeyasinghe, R.R et al. “National Malaria Control Programme of Sri Lanka.” Asia Pacific Malaria Elimination Network, n.d. Web. 2 August 2011. <http://apmen.org/storage/country-partner/Sri%20Lanka%20-%20Strategic%20Plan%20for%20Phased%20Elimination.pdf>
Bräutigam, Deborah A. and Stephen Knack. “Foreign Aid, Institutions, and Governance in Sub-Saharan Africa.” Economic Development and Cultural Change. 52.2 (2004): 255-285. Web. 11 Apr 2011. <http://www.jstor.org/pss/10.1086/380592>
Clardy, Jon, Michael Fischbach, and Cameron Currie. “The natural history of antibiotics.” Current Biology 19.11 (2009). Web. 2 August 2011. <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2731226/?tool=pubmed>
Collier, Paul. The Bottom Billion: Why the Poorest Countries Are Failing and What Can Be Done About It. New York: Oxford University Press, 2007. Book.
Espinal, Marcos A et al. “Global Trends in Resistance to Anti-Tuberculosis Drugs.” New England Journal of Medicine 344.17 (2001). Web. 20 Apr 2011. <http://www.nejm.org/doi/pdf/10.1056NEJM200104263441706>
Haak, Hilbrand, and Aryanti Radyowijati. “Improving antibiotic use in low-income countries: an overview of evidence on determinants.” ScienceDirect. 57.4 (2003): 733-744. Web. 23 Feb 2011. <http://archives.who.int/icium/icium2004/resources/ppt/AM020.pdf>
Health, Statistics, and Informatics Department, Causes of Death 2008 Summary Tables, World Health Organization, May 2011, Web, AFR and AMR tables, row U020.
Honrado, E.R et al. “Cost-effectiveness analysis of artesunate and quinine + tetracycline for the treatment of uncomplicated falciparum malaria in Chanthaburi, Thailand.” Bulletin of the World Health Organization 77.3 (1999): 235-243. Web. 2 August 2011.
Hotez, Peter J, and Aruna Kamath. “Neglected Tropical Diseases in Sub-Saharan Africa: Review of Their Prevalence, Distribution, and Disease Burden.” Neglected Tropical Diseases 3.8 (2009): 412. Web. 27 Mar 2011.<http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2727001/?tool=pubmed >
Lumumba-Kasongo, Tukumbi. “Reconceptualizing the State as the Leading
Agent of Development in the Context of Globalization in Africa African Journal of Political Science 7.1 (2002):79-108. Web. 27 Feb 2011. <http://digital.lib.msu.edu/projects/africanjournals/pdfs/volume7n1.pdf>
Narasimhan, Vasant and Amir Attaran. “Roll Back Malaria? The scarcity of international aid for malaria control.” Malaria Journal 2.8 (2003). 20 Apr 2011.
Rao, Chalapati, Alan D Lopez, and Yusuf Hemed. “Chapter 5: Causes of Death.” Disease and Mortality in Sub-Saharan Africa (2006): n. pag. Web. 20 Apr 2011.
Sachs, Jeffrey, and Pia Malaney. “The economic and social burden of malaria.” Nature 415 (2002): 680-685. Web. 1 April 2011. <http://www.nature.com/nature/journal/v415/n6872/full/415680a.html?lang=e>
Tanner, Marcel and Savigny, Don de. Malaria eradication back on the table. Bulletin of the World Health Organization 86.2 (2008): 82. <http://www.scielosp.org/scielo.php?script=sci_arttext&pid=S0042-96862008…. ISSN 0042-9686. doi: 10.1590/S0042-96862008000200002.
“Chapter 1: Why the MDG’s are important, where we stand, and why we’re falling short.” Millenium Project Main Report. United Nations Millennium Project. Web. 11 Apr 2011. < http://www.unmillenniumproject.org/documents/MainReportChapter1-lowres.pdf>
“How Many Children in Africa Reach Secondary Education.” UNESCO Fact Sheet. UNESCO Institute for Statistics. Web. 1 Apr. 2011. <http://www.uis.unesco.org/TEMPLATE/pdf/EducGeneral/UIS_Fact%20Sheet_2006>
“World Health Organization Statistics.” Health-related Millennium Development Goals. World Health Organization. Web. 20 Apr 2011. <http://www.who.int/whosis/whostat/EN_WHS10_Part1.pdf>
World Bank Data. The World Bank, 2011. Web. 2 August 2011.
